
In recent years, artificial intelligence has emerged as a transformative force in healthcare, revolutionizing how diseases are diagnosed, treatments are developed, and patient care is delivered. The integration of AI technologies into medical practice represents one of the most significant paradigm shifts in modern medicine, promising more accurate diagnoses, personalized treatment plans, and improved patient outcomes. This article explores the recent breakthroughs in AI applications for healthcare diagnostics and personalized medicine, examining their impact, challenges, and future potential.
The Evolution of AI in Healthcare
The journey of AI in healthcare began decades ago with rule-based expert systems attempting to mimic clinical decision-making. However, recent advancements in machine learning, particularly deep learning, have catapulted AI capabilities to unprecedented heights. Today’s healthcare AI systems can analyze vast amounts of complex medical data—from medical images and electronic health records to genomic sequences and lifestyle information—identifying patterns that might escape even the most experienced clinicians.
By 2024, the global AI in healthcare market had reached approximately $45.2 billion, with projections suggesting it could exceed $187 billion by 2030. This remarkable growth reflects the increasing recognition of AI’s potential to address critical challenges in healthcare delivery, including diagnostic errors, treatment inefficiencies, and the growing burden of chronic diseases.
Diagnostic Breakthroughs
Medical Imaging Revolution
Perhaps the most visible impact of AI in healthcare has been in medical imaging diagnostics. Advanced neural networks, particularly convolutional neural networks (CNNs), have demonstrated remarkable abilities in analyzing radiological images, often matching or exceeding human performance.
Radiology
In radiology, AI systems now routinely assist in detecting and characterizing abnormalities across various imaging modalities:
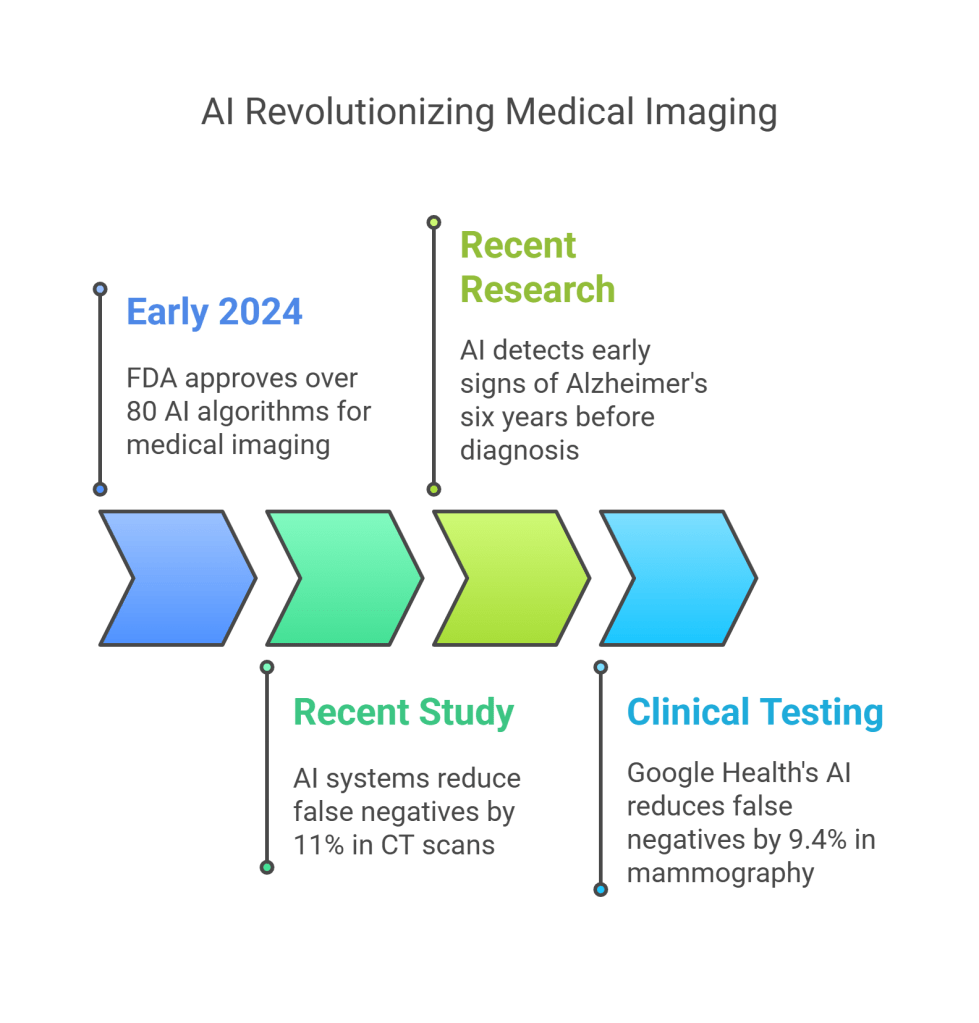
CT Scans: AI algorithms can detect early signs of lung cancer with sensitivity rates exceeding 94%, often identifying nodules too small for human radiologists to notice. A landmark study published in Nature Medicine demonstrated that AI systems reduced false negatives by 11% and false positives by 5% compared to experienced radiologists working alone.
MRI Analysis: Deep learning models have transformed brain MRI interpretation, enabling more precise delineation of tumors and early detection of neurodegenerative conditions. Recent research has shown AI systems capable of detecting early signs of Alzheimer’s disease from MRI scans up to six years before clinical diagnosis, potentially allowing for earlier intervention.
Mammography: AI-enhanced breast cancer screening has shown remarkable progress, with systems like Google Health’s mammography AI reducing false negatives by 9.4% and false positives by 5.7% in clinical testing. These improvements are particularly significant given that breast cancer remains one of the leading causes of cancer death among women globally.
The FDA has accelerated approvals for AI-based medical imaging tools, with over 80 algorithms receiving clearance by early 2024. These tools are increasingly integrated into clinical workflows, serving as “second readers” that enhance radiologists’ efficiency and accuracy rather than replacing them.
Pathology
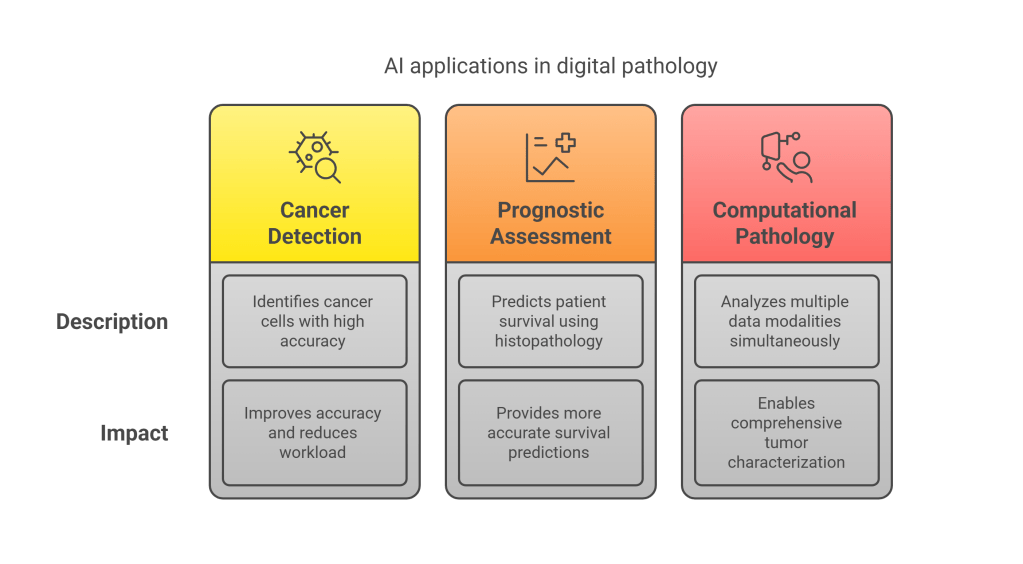
Digital pathology has similarly witnessed an AI revolution. Machine learning algorithms now assist pathologists in analyzing tissue samples with unprecedented precision:
Cancer Detection: AI systems can identify cancer cells with accuracy rates approaching 99% in certain applications. For instance, algorithms analyzing prostate biopsies have demonstrated Gleason score classifications that rival consensus diagnoses from expert pathologists.
Prognostic Assessment: Beyond detection, AI tools provide valuable prognostic information. A 2023 study in Nature Communications showed that deep learning analysis of histopathology slides could predict patient survival more accurately than traditional staging methods for multiple cancer types.
Computational Pathology: The integration of molecular data with digital pathology images has given rise to computational pathology, where AI systems analyze multiple data modalities simultaneously. This holistic approach allows for more comprehensive tumor characterization and more precise treatment targeting.
The impact of these advances extends beyond improved accuracy. By automating routine aspects of image analysis, AI enables pathologists to focus on complex cases requiring human expertise, potentially alleviating bottlenecks in pathology workflows as cancer screening programs expand globally.
Early Disease Detection
AI systems are increasingly capable of detecting diseases before clinical symptoms appear, potentially transforming the paradigm from reactive to preventive care:
Retinal Imaging: AI analysis of retinal images can now predict cardiovascular risk factors without requiring blood tests. Google’s DeepMind demonstrated that neural networks examining retinal scans could predict cardiovascular events with accuracy comparable to current clinical methods. The retina’s unique position as the only place where blood vessels can be directly observed non-invasively makes it an invaluable window into systemic health.
Voice Analysis: Voice-based AI diagnostic tools can detect subtle changes in speech patterns associated with various conditions. For example, algorithms analyzing voice recordings can identify Parkinson’s disease with over 90% accuracy up to five years before clinical diagnosis, by detecting minute changes in vocal tremor and rhythm.
Wearable Data Integration: AI systems analyzing data from consumer wearables have made significant strides in early detection. Apple Watch’s irregular rhythm notification feature, validated in the Apple Heart Study involving over 400,000 participants, has demonstrated the ability to identify atrial fibrillation with a positive predictive value of 84%, potentially preventing strokes through early intervention.
Liquid Biopsies: AI is enhancing the sensitivity and specificity of liquid biopsy tests, which detect circulating tumor DNA in blood samples. GRAIL’s Galleri test, which employs machine learning to analyze cell-free DNA methylation patterns, can detect over 50 cancer types with a false positive rate under 1%, potentially enabling earlier treatment when interventions are most effective.
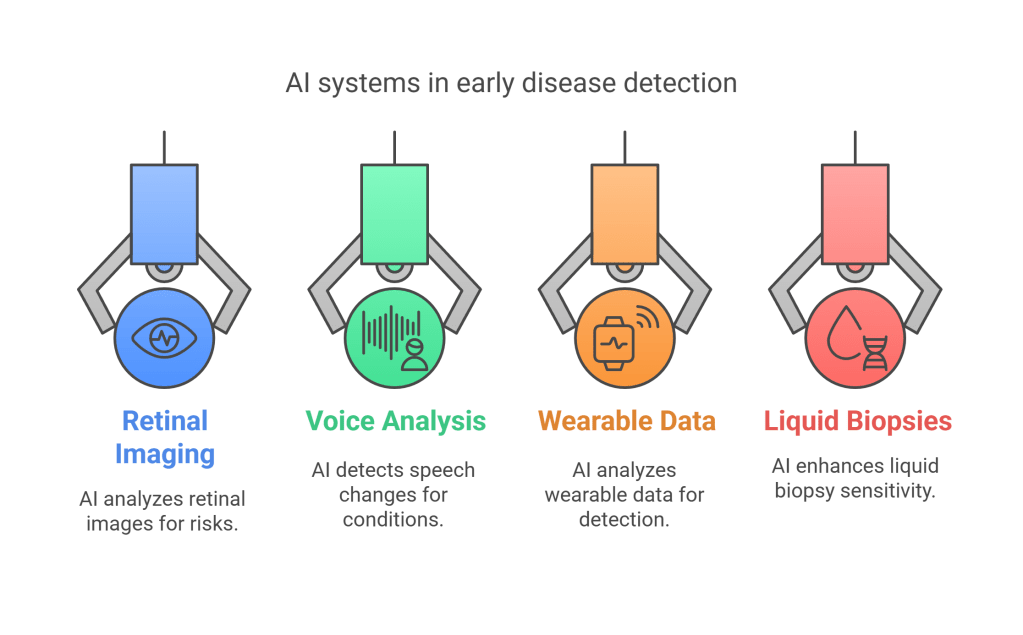
These early detection capabilities represent one of AI’s most promising contributions to healthcare, potentially shifting the balance from late-stage disease management to early intervention and prevention.
Diagnostics in Resource-Limited Settings
AI diagnostic tools hold particular promise for regions with limited healthcare infrastructure and shortages of specialists:
Smartphone-Based Diagnostics: Machine learning applications that work on smartphones can bring specialist-level diagnostics to remote areas. For instance, the IDx-DR system, which analyzes retinal images for diabetic retinopathy, allows primary care providers to screen patients without requiring an ophthalmologist, achieving sensitivity and specificity exceeding 90%.
Point-of-Care Applications: AI-enabled diagnostic devices are increasingly deployed at the point of care in low-resource settings. An example is the automated microscopy system developed by Motic and Global Good, which uses deep learning to identify malaria parasites in blood smears with accuracy comparable to expert microscopists but at a fraction of the time and cost.
Teleconsultation Enhancement: AI tools are enhancing telemedicine capabilities in underserved areas by pre-analyzing patient data and images before specialist review. This approach, demonstrated in projects like the Peek Vision platform for eye diseases, enables more efficient use of scarce specialist time while expanding access to quality care.

By reducing dependence on specialists and expensive equipment, these AI applications could help address the critical shortage of healthcare professionals affecting many regions, potentially democratizing access to high-quality diagnostics.
Personalized Medicine Revolution
While diagnostic advances have garnered significant attention, perhaps the most profound impact of AI in healthcare lies in its ability to personalize treatment approaches to individual patients.

Genomic Medicine and AI
The convergence of genomic sequencing and AI analysis has accelerated the promise of truly personalized medicine:
Variant Interpretation: Deep learning algorithms now assist in interpreting genomic variants, determining which mutations may drive disease and which are benign. Google’s DeepVariant, which won the PrecisionFDA Truth Challenge, demonstrates how AI can improve the accuracy of genetic variant calling from sequencing data.
Pharmacogenomics: AI systems can predict how genetic variations influence drug responses, enabling more precise medication selection and dosing. For example, algorithms analyzing genomic data can now predict with over 90% accuracy which leukemia patients will respond to specific chemotherapy regimens, potentially sparing non-responders from unnecessary toxicity.
Gene-Environment Interactions: Machine learning models increasingly incorporate both genetic and environmental data to provide more holistic risk assessments. The eMERGE Network has demonstrated how AI can integrate genomic information with electronic health records to improve risk prediction for conditions ranging from atrial fibrillation to type 2 diabetes.
As sequencing costs continue to decline—dropping below $200 for whole genome sequencing by 2024—and AI interpretation improves, genomic medicine is becoming increasingly accessible and clinically relevant.
Treatment Selection and Optimization
AI systems are transforming treatment planning across medical specialties:
Oncology: Precision oncology has been revolutionized by AI tools that match cancer patients to optimal treatments based on their tumor’s genetic profile. IBM’s Watson for Oncology analyzes patients’ medical information against a vast database of medical literature and clinical trials to recommend evidence-based treatment options. More advanced systems now incorporate additional data points, including immune markers, microbiome profiles, and imaging characteristics, to further refine treatment selection.
Chronic Disease Management: For chronic conditions like diabetes, AI algorithms analyze continuous glucose monitoring data alongside lifestyle information to provide personalized management recommendations. Studies have shown that AI-guided insulin dosing can improve time in target glucose range by over 20% compared to standard approaches.
Neurology: In epilepsy management, machine learning models analyze electroencephalogram (EEG) data to predict seizures hours before they occur, allowing for preemptive intervention. These systems achieve prediction accuracy exceeding 85% in some patient populations, potentially transforming quality of life for those with refractory epilepsy.
Psychiatry: AI-driven approaches to mental health treatment selection show particular promise in a field where treatment response is notoriously variable. Algorithms analyzing brain imaging, genetic markers, and symptom patterns can now predict with approximately 75% accuracy which depression patients will respond to specific antidepressants, potentially reducing the trial-and-error approach that characterizes current practice.

The common thread across these applications is the shift from population-based treatment approaches to truly individualized care plans that consider the unique characteristics of each patient.
Drug Discovery and Development
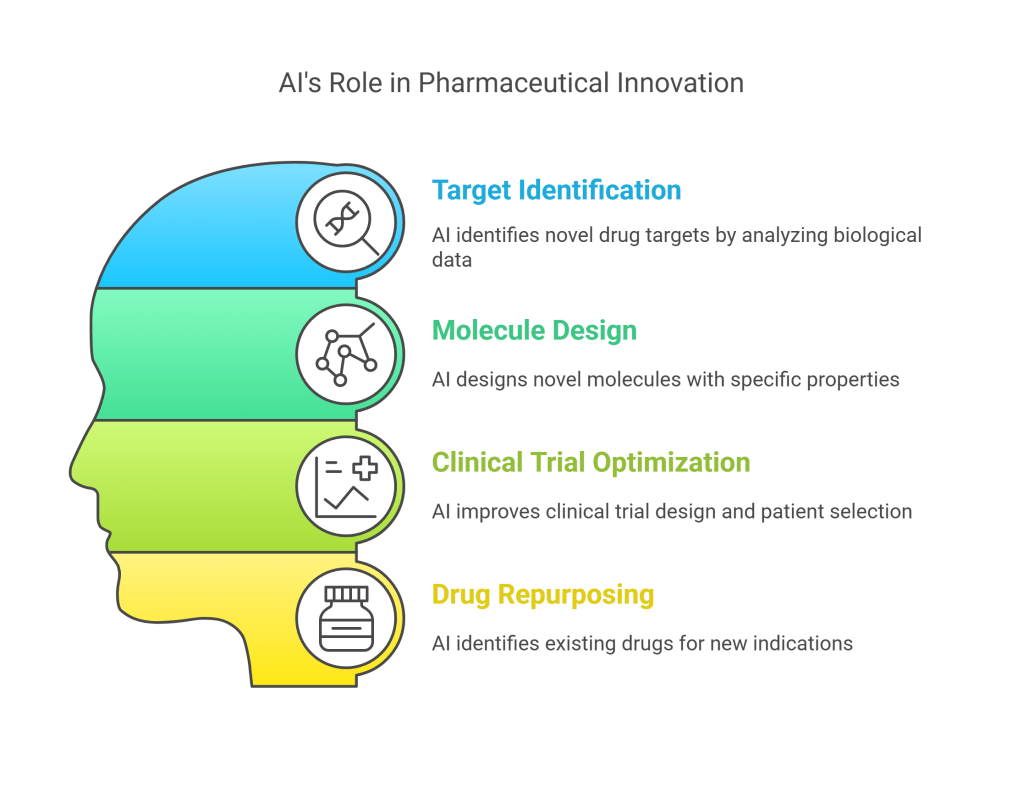
AI is dramatically accelerating pharmaceutical research and development:
Target Identification: Machine learning algorithms analyze biological data to identify novel drug targets. For example, BenevolentAI’s platform identified baricitinib as a potential COVID-19 treatment by analyzing its ability to disrupt receptor-mediated endocytosis, a critical viral entry mechanism. Clinical trials subsequently confirmed its efficacy, leading to FDA emergency use authorization.
Molecule Design: Generative models can now design novel molecules with specific properties. Insilico Medicine’s AI platform designed, synthesized, and preclinically validated a novel drug candidate for idiopathic pulmonary fibrosis in just 18 months, compared to the typical 3-5 years required using traditional methods.
Clinical Trial Optimization: AI systems improve clinical trial design by identifying biomarkers for patient stratification and predicting which patients are most likely to respond to experimental treatments. Unlearn.AI has developed “digital twins”—AI-generated synthetic control patients based on real patient data—that could reduce the number of placebo recipients required in clinical trials while maintaining statistical power.
Drug Repurposing: Machine learning approaches have accelerated drug repurposing efforts by identifying existing medications that might be effective for new indications. The COVID-19 pandemic highlighted this capability, with AI systems helping to identify dexamethasone and other existing drugs as effective treatments months before traditional clinical research could establish their efficacy.
These AI-driven approaches are helping address the pharmaceutical industry’s productivity challenge, where traditional R&D costs have risen to approximately $2.6 billion per approved drug while success rates have declined.
Clinical Implementation and Real-World Impact
While research breakthroughs generate headlines, the real test of AI’s value lies in successful clinical implementation and measurable improvements in patient outcomes.
Integration into Clinical Workflows
Healthcare AI tools are increasingly moving beyond research environments into routine clinical practice:
Electronic Health Record Integration: Leading EHR vendors have incorporated AI capabilities directly into their platforms. Epic’s Cognitive Computing platform includes machine learning models that identify patients at risk for conditions ranging from sepsis to readmission, while Cerner’s HealtheDataLab enables health systems to develop and deploy custom AI algorithms within existing workflows.
Clinical Decision Support: AI-powered clinical decision support systems now provide real-time guidance during patient encounters. Mayo Clinic’s collaboration with Google has produced AI tools that assist emergency department physicians in diagnosing cardiac conditions from ECG data, reducing time to treatment for high-risk patients.
Ambient Clinical Intelligence: Natural language processing systems that automatically document patient encounters are gaining traction. Nuance’s Dragon Ambient eXperience (DAX), which transcribes and organizes clinic visits into structured notes, has been shown to reduce physician documentation time by 50% while improving note quality and patient satisfaction.
Successful implementations typically approach AI as augmenting rather than replacing clinician judgment, addressing specific workflow pain points while carefully managing the change management challenges inherent in healthcare innovation.
Patient Outcomes and System Efficiency
Early evidence suggests that well-implemented healthcare AI can deliver meaningful improvements in outcomes and efficiency:
Mortality Reduction: At Geisinger Health System, an AI system analyzing EHR data to identify patients at risk of sepsis reduced mortality by 18.2% when deployed across emergency departments and hospitals. The system’s sensitivity (82%) and specificity (85%) represented significant improvements over existing sepsis screening protocols.
Length of Stay Reduction: Mount Sinai’s AI-driven “Hospital at Home” program, which uses predictive analytics to identify patients who can safely receive hospital-level care at home, has reduced costs by 38% while decreasing readmissions by 7% compared to traditional inpatient care.
Resource Optimization: Providence St. Joseph Health’s AI-powered patient flow system has improved operating room utilization by 16% and reduced emergency department boarding times by 25% by optimizing scheduling and predicting capacity needs.
Diagnostic Accuracy: A multi-center study of an AI system for colonoscopy polyp detection showed a 30% increase in adenoma detection rate when the system assisted gastroenterologists, potentially translating to significant reductions in interval colorectal cancers.
These early successes suggest that AI can help address the healthcare “quadruple aim” of improving population health, enhancing patient experience, reducing costs, and improving clinician work life.
Challenges and Ethical Considerations
Despite remarkable progress, significant challenges remain in realizing the full potential of AI in healthcare diagnostics and personalized medicine.

Data Quality and Accessibility
AI systems require high-quality, representative data for development and validation:
Data Fragmentation: Healthcare data remains siloed across different providers, systems, and formats, limiting the comprehensiveness of AI training datasets. Initiatives like the FHIR (Fast Healthcare Interoperability Resources) standard are addressing this issue, but widespread interoperability remains elusive.
Bias and Representativeness: Many medical datasets overrepresent certain populations while underrepresenting others. This imbalance has led to documented biases in AI systems—for example, dermatology algorithms showing lower accuracy for darker skin tones and cardiovascular risk models underperforming in women and minority populations.
Privacy and Security: The sensitive nature of healthcare data necessitates robust privacy protections, which can create tensions with data sharing needs for AI development. Federated learning approaches, which allow algorithms to be trained across multiple institutions without centralizing patient data, represent a promising solution but add technical complexity.
Addressing these data challenges requires not only technical innovations but also policy changes and stakeholder collaboration across the healthcare ecosystem.
Validation and Regulatory Considerations
Bringing AI healthcare tools from laboratory to clinical use requires navigating complex validation and regulatory landscapes:
Real-World Validation: Many AI systems demonstrate impressive performance in controlled research environments but struggle to maintain that performance when deployed in diverse clinical settings. The FDA’s Digital Health Software Precertification Program represents an attempt to create more flexible regulatory frameworks for continuously learning AI systems.
Reference Standards: Establishing appropriate “ground truth” for AI evaluation can be challenging, particularly when expert opinions differ or gold standard diagnostics are impractical. The concept of “non-inferiority” to human experts has emerged as one pragmatic approach to AI validation.
Regulatory Evolution: Regulatory frameworks continue to evolve to accommodate AI’s unique characteristics. The FDA’s proposed regulatory framework for AI/ML-based software as a medical device (SaMD) acknowledges the need for mechanisms to evaluate algorithm changes after initial approval, addressing the “adaptive” nature of many healthcare AI systems.
As AI systems become more autonomous and consequential in healthcare decision-making, establishing appropriate validation standards and regulatory oversight becomes increasingly critical.
Clinical Integration and Human Factors
Technical excellence alone does not ensure successful clinical adoption:
Clinician Trust and Acceptance: Healthcare professionals vary in their willingness to incorporate AI recommendations into clinical practice. Explainable AI approaches, which provide interpretable rationales for AI conclusions, have shown promise in building clinician trust and facilitating appropriate reliance on AI systems.
Workflow Integration: AI tools that add steps to already complex clinical workflows face significant adoption barriers. The most successful implementations integrate seamlessly into existing processes, minimizing additional cognitive burden on healthcare providers.
Liability and Responsibility: Questions about who bears responsibility when AI-assisted decisions lead to adverse outcomes remain complex and largely unresolved. Professional society guidelines, such as those from the American College of Radiology, increasingly address appropriate use of AI tools, but legal and ethical frameworks continue to evolve.
Health Equity Impacts: Without careful implementation, AI could exacerbate rather than mitigate healthcare disparities. Proactive approaches to algorithmic fairness, inclusive design processes, and continuous monitoring for disparate impacts are essential to ensure AI benefits all patient populations equitably.
The sociotechnical nature of healthcare means that successful AI implementation requires attention to human, organizational, and social factors alongside technical development.
Future Directions
Looking ahead, several emerging trends are likely to shape the continued evolution of AI in healthcare diagnostics and personalized medicine.
Multimodal Integration
Future AI systems will increasingly integrate data from multiple sources to provide more comprehensive insights:
Integrated Diagnostics: By analyzing pathology, radiology, genomic, and clinical data simultaneously, multimodal AI systems promise more accurate and comprehensive disease characterization. Early examples include systems that combine histopathology images with genomic data to more precisely classify cancer subtypes and predict treatment response.
Digital Twins: The concept of patient-specific “digital twins”—computational models that simulate an individual’s physiology and potential response to interventions—is gaining momentum. These models, incorporating imaging, -omics, and real-time monitoring data, could enable virtual testing of treatment options before actual administration.
Ambient Intelligence: Healthcare environments equipped with sensors, cameras, and microphones processed by AI could provide continuous, passive monitoring of patient status. Early applications in intensive care units have demonstrated the ability to predict deterioration events hours before conventional monitoring systems detect problems.
These integrative approaches acknowledge the multifactorial nature of health and disease, potentially capturing interactions between different physiological systems that might be missed by single-modality analyses.
Decentralized and Democratic AI
AI capabilities are increasingly extending beyond traditional healthcare settings:
Edge Computing: AI algorithms deployed on edge devices—from smartphones to bedside monitors—eliminate reliance on cloud connectivity, enabling real-time analysis in remote or resource-limited settings. This approach has shown particular promise in applications like continuous arrhythmia monitoring and seizure detection.
Patient-Directed Tools: AI applications designed for direct patient use are proliferating, from symptom checkers to medication adherence support. These tools potentially empower patients to play more active roles in their health management while extending the reach of healthcare systems.
Open Source Healthcare AI: Community-driven initiatives like MONAI (Medical Open Network for AI) are democratizing access to healthcare AI tools and frameworks, potentially accelerating innovation and reducing disparities in AI development capabilities across institutions and regions.
These trends reflect a broader shift toward more distributed healthcare delivery models, with AI potentially serving as a bridge between traditional clinical settings and everyday life.
Precision Public Health
AI’s impact is expanding from individual patient care to population health management:
Disease Surveillance: Machine learning systems analyzing diverse data streams—from social media posts to wastewater sampling—have demonstrated remarkable abilities to detect disease outbreaks earlier than traditional surveillance systems. During the COVID-19 pandemic, AI-powered wastewater monitoring provided early warnings of case surges up to two weeks before clinical testing data reflected increased transmission.
Population Risk Stratification: AI models incorporating social determinants of health alongside clinical data enable more precise identification of high-risk populations. In diabetes prevention, models incorporating neighborhood characteristics, food accessibility, and socioeconomic factors alongside clinical risk factors have improved the precision of intervention targeting by over 30%.
Resource Allocation Optimization: During public health emergencies, AI systems can optimize the distribution of limited resources. For example, during vaccine rollouts, machine learning models helped prioritize distribution to maximize population impact while considering both biological vulnerability and access barriers.
These applications suggest AI’s potential to help address not only individual health outcomes but also broader public health challenges and health disparities.
Conclusion
The integration of AI into healthcare diagnostics and personalized medicine represents one of the most promising developments in modern medicine. From improving diagnostic accuracy and enabling earlier disease detection to personalizing treatment selection and accelerating drug development, AI technologies are transforming every aspect of the healthcare continuum.
Despite significant challenges—including data quality issues, regulatory complexities, and implementation barriers—the trajectory is clear. Healthcare is moving from a standardized, reactive approach toward a more personalized, proactive paradigm enabled by artificial intelligence. The future healthcare landscape will likely feature an increasingly seamless partnership between human expertise and machine intelligence, combining the contextual understanding and empathy of healthcare professionals with the pattern recognition capabilities and tireless consistency of AI systems.
For this future to fully materialize in ways that benefit all patients equitably, continued attention to ethical implementation, rigorous validation, and thoughtful integration into clinical workflows will be essential. With these considerations in mind, AI has the potential to help realize the long-promised vision of truly personalized medicine—delivering the right care to the right patient at the right time, ultimately improving outcomes while potentially reducing costs and enhancing both patient and provider experiences.
Discover more from SkillWisor
Subscribe to get the latest posts sent to your email.
